Table of Contents
Keep in mind: The complying with criteria use to grownups, adolescents, and children older than 6 years. For children 6 years and younger, see the DSM-5 area labelled "Posttraumatic Stress Disorder for Kid 6 Years (even more ...) Michael is a 62-year-old Vietnam expert. He is a separated father of 2 youngsters and has four grandchildren.
His dad literally and mentally abused him (e.g., he was beaten with a button up until he had welts on his legs, back, and buttocks). By age 15, he was making use of marijuana, hallucinogens, and alcohol and was frequently truant from school.
Eye Movement Desensitization and Reprocessing Intensives: How You Should Know
In one incident, the soldier he was beside in a bunker was shot. Michael really felt defenseless as he spoke to this soldier, who was still mindful. In Vietnam, Michael boosted his use both alcohol and marijuana. On his go back to the United States, Michael remained to drink and utilize cannabis.
His life supported in his very early 30s, as he had a constant job, supportive buddies, and a reasonably secure household life. Quickly thereafter, he married a second time, but that marriage ended in separation.
Why Select EMDR over Accelerated Resolution Therapy to treat Personal Situation
In the 1980s, Michael obtained a number of years of psychological health and wellness treatment for dysthymia. In the mid-1990s, he returned to outpatient therapy for comparable signs and symptoms and was detected with PTSD and dysthymia.
He reported that he really did not like just how alcohol or other materials made him really feel anymorehe really felt out of control with his emotions when he utilized them. Michael reported symptoms of hyperarousal, breach (intrusive memories, headaches, and busying ideas concerning Vietnam), and evasion (separating himself from others and feeling "numb"). He reported that these symptoms seemed to connect to his childhood years abuse and his experiences in Vietnam.
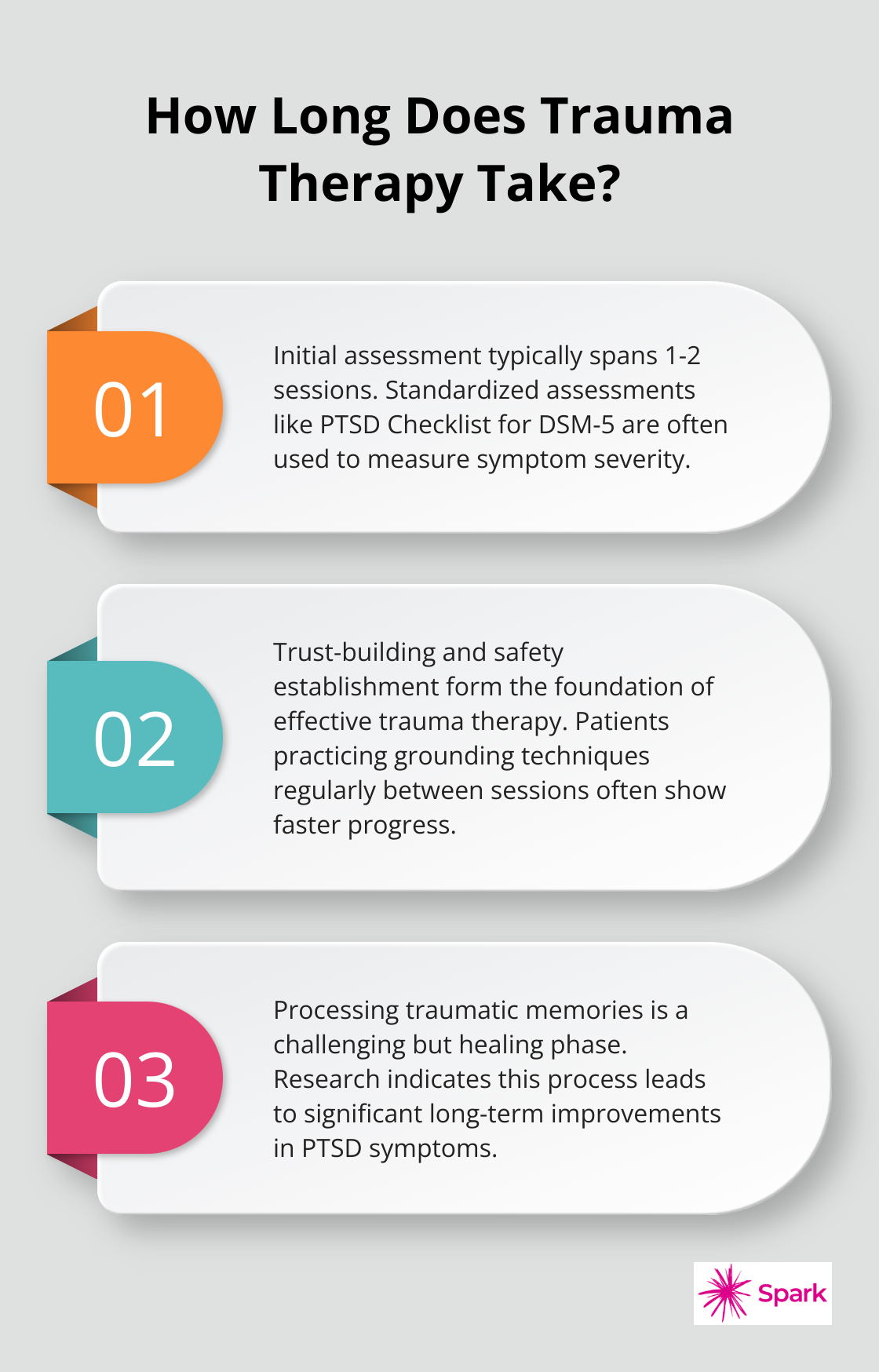
Processing PTSD through Evidence-Based Therapeutic Approaches
Seeing a movie regarding child abuse can set off symptoms connected to the trauma. Various other triggers include returning to the scene of the injury, being advised of it in a few other means, or noting the anniversary of an event. Combat professionals and survivors of community-wide catastrophes may seem to be coping well shortly after an injury, just to have symptoms arise later on when their life circumstances seem to have actually stabilized.
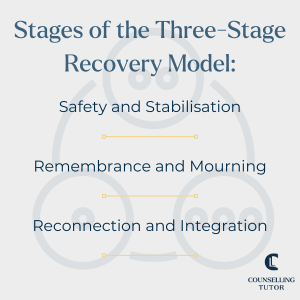
Draw a connection in between the trauma and providing trauma-related signs and symptoms. Understand that triggers can come before terrible anxiety reactions, consisting of delayed actions to trauma. Develop coping strategies to browse and manage signs and symptoms.
Payment & Investment Options regarding EMDR
It would be perceived as unacceptable and potentially bastardizing to focus on the psychological distress that he or she still births. (For an evaluation of cultural proficiency in treating trauma, refer to Brown, 2008.)Methods for determining PTSD are additionally culturally specific. As part of a project started in 1972, the World Health Company (THAT) and the National Institutes of Health And Wellness (NIH) started a joint research study to evaluate the cross-cultural applicability of category systems for different medical diagnoses.
Thus, it's usual for injury survivors to be underdiagnosed or misdiagnosed. If they have not been determined as trauma survivors, their emotional distress is often not connected with previous trauma, and/or they are identified with a disorder that marginally matches their presenting signs and psychological sequelae of injury. The complying with areas present a brief review of some mental disorders that can arise from (or be gotten worse by) traumatic stress and anxiety.
The term "co-occurring problems" refers to situations when a person has one or more mental illness as well as one or even more compound usage disorders (including chemical abuse). Co-occurring conditions are typical among people that have a history of trauma and are looking for aid. Just people particularly educated and accredited in mental wellness evaluation need to make medical diagnoses; injury can result in challenging cases, and lots of symptoms can be present, whether or not they satisfy full diagnostic criteria for a certain disorder.
Much more study is currently analyzing the numerous prospective paths among PTSD and various other problems and just how various sequences impact medical discussion. TIP 42, Chemical Abuse Treatment for Individuals With Co-Occurring Conditions (CSAT, 2005c), is beneficial in understanding the relationship important use to various other mental illness. There is plainly a connection in between trauma (consisting of private, group, or mass trauma) and material make use of along with the presence of posttraumatic anxiety (and various other trauma-related problems) and substance make use of problems.
Which People Benefits with EMDR Therapy and ART Treatment specializing in Trauma therapy
Furthermore, individuals with material usage disorders go to greater danger of establishing PTSD than people that do not abuse substances. Counselors collaborating with trauma survivors or customers who have material usage disorders need to be especially familiar with the possibility of the various other condition arising. Individuals with PTSD usually have at the very least one added diagnosis of a mental illness.
There is a risk of misunderstanding trauma-related signs basically misuse therapy settings. Evasion symptoms in a specific with PTSD can be misunderstood as lack of inspiration or hesitation to involve in material abuse therapy; a therapist's initiatives to address substance abuserelated behaviors in early recovery can also prompt an overstated feedback from an injury survivor that has profound terrible experiences of being caught and controlled.
PTSD and Material Use Disorders: Vital Treatment Truths. PTSD is among one of the most typical co-occurring mental disorders discovered in clients in substance abuse treatment (CSAT, 2005c). Individuals in treatment for PTSD often tend to abuse a variety of compounds, (even more ...) Maria is a 31-year-old woman diagnosed with PTSD and alcohol reliance.
Navigation
Latest Posts
Digital Tools in Trauma Therapy Care
Parent Partnership in Child Adult Assessment Services
Attention Deficit Assessment That Goes Beyond Behavioral Surveys